How ecstasy and psilocybin are shaking up psychiatry
Nature, 2021, 589, 506-509
d41586-021-00187-9

Illustration by Gizem Vural
On a sunny day in London in 2015, Kirk Rutter rode the Tube to Hammersmith Hospital in hopes of finally putting an end to his depression.
Rutter had lived with the condition off and on for years, but the burden had grown since the death of his mother in 2011, followed by a relationship break-up and a car accident the year after. It felt as if his brain was stuck on what he describes as “an automatic circuit”, repeating the same negative thoughts like a mantra: “‘Everything I do turns to crap.’ I actually believed that,” he recalls.
The visit to Hammersmith was a preview. He would be returning the next day to participate in a study, taking a powerful hallucinogen under the guidance of Robin Carhart-Harris, a psychologist and neuroscientist at Imperial College London. Years of talking therapy and a variety of anti-anxiety medications had failed to improve Rutter’s condition, qualifying him for the trial.
“Everyone was super nice, like really lovely, and especially Robin,” Rutter recalls. Carhart-Harris led him to a room with a magnetic resonance imaging (MRI) machine, so researchers could acquire a baseline of his brain activity. Then he showed Rutter where he would spend his time while on the drug. Carhart-Harris asked him to lie down and played him some of the music that would accompany the session. He explained that he would have on hand a drug that could neutralize the hallucinogen, if necessary. Then the two practised a grounding technique, to help calm Rutter in the event that he became overwhelmed. Without warning, Rutter burst into tears.
“I think I knew this was going to be unpacking a lot — I was carrying a bit of a load at the time,” Rutter says.
When Rutter returned the next day, one of the researchers handed him two pills containing a synthetic form of psilocybin, the psychoactive ingredient found in magic mushrooms. Rutter lay down on the bed and put on headphones and an eye mask. Soon, images of Sanskrit text appeared to him. Later, he saw golden bejewelled structures. Then his mind went to work on his grief.
The Imperial study was one of a spate of clinical trials launched over the past few years using illicit psychedelic drugs such as psilocybin, lysergic acid diethylamide (LSD) and MDMA (3,4-methylenedioxymethamphetamine, also known as molly or ecstasy) to treat mental-health disorders, generally with the close guidance of a psychiatrist or psychotherapist. The idea has been around for decades — or centuries in some cultures — but the momentum has picked up drastically over the past few years as investors and scientists have begun to champion the approach again (see ‘Psychedelics take flight’).
Source: Dimensions
Once dismissed as the dangerous dalliances of the counterculture, these drugs are gaining mainstream acceptance. Several states and cities in the United States are in the process of legalizing or decriminalizing psilocybin for therapeutic or recreational purposes. And respected institutions such as Imperial; Johns Hopkins University in Baltimore, Maryland; the University of California, Berkeley; and the Icahn School of Medicine at Mount Sinai in New York City have opened centres devoted to studying psychedelics. Several small studies suggest the drugs can be safely administered and might have benefits for people with intractable depression and other psychological problems, such as post-traumatic stress disorder (PTSD). One clinical trial involving MDMA has recently ended, with results expected to be published soon. Regulators will then be considering whether to make the treatment available with a prescription.
Psychedelic-assisted psychotherapy could provide needed options for debilitating mental-health disorders including PTSD, major depressive disorder, alcohol-use disorder, anorexia nervosa and more that kill thousands every year in the United States, and cost billions worldwide in lost productivity.
But the strategies represent a new frontier for regulators. “This is unexplored ground as far as a formally evaluated intervention for a psychiatric disorder,” says Walter Dunn, a psychiatrist at the University of California, Los Angeles, who sometimes advises the US Food and Drug Administration (FDA) on psychiatric drugs. Most drugs that treat depression and anxiety can be picked up at a neighbourhood pharmacy. These new approaches, by contrast, use a powerful substance in a therapeutic setting under the close watch of a trained psychotherapist, and regulators and treatment providers will need to grapple with how to implement that safely.
“The clinical trials that have been reported on depression have been done under highly circumscribed and controlled conditions,” says Bertha Madras, a psychobiologist at Harvard Medical School who is based at McLean Hospital in Belmont, Massachusetts. That will make interpreting results difficult. A treatment might show benefits in a trial because the experience is carefully coordinated, and everyone is well trained. Placebo controls pose another challenge because the drugs have such powerful effects.
And there are risks. In extremely rare instances, psychedelics such as psilocybin and LSD can evoke a lasting psychotic reaction, more often in people with a family history of psychosis. Those with schizophrenia, for example, are excluded from trials involving psychedelics as a result. MDMA, moreover, is an amphetamine derivative, so could come with risks for abuse.
But many researchers are excited. Several trials show dramatic results: in a study published in November 2020, for example, 71% of people who took psilocybin for major depressive disorder showed a greater than 50% reduction in symptoms after four weeks, and half of the participants entered remission1. Some follow-up studies after therapy, although small, have shown lasting benefits2,3.
“Sometimes with a therapeutic, you look at the data and think, ‘It slightly moved the needle,’” says Jennifer Mitchell, a neurologist at the Weill Institute for Neurosciences at the University of California, San Francisco, who worked on the recently finished MDMA trial. “Then you see MDMA and you’re like, ‘Never mind that.’ It’s a very different effect size.” Rutter was so moved by his experience with psilocybin that he has consulted for one of the companies sponsoring trials of the compound.
Rave new world
The current wave of interest in the therapeutic potential of psychedelics is something of a renaissance. In the 1950s and 1960s, scientists published more than 1,000 articles on using psychedelics as a psychiatric treatment; the drugs were tested on around 40,000 people in total4. Then, as recreational use of the drugs spread, they were banned and the FDA constricted supplies for research. Only recently have neuroscientists and psychopharmacologists such as Carhart-Harris had the technology to start unpicking how they work in the brain. That has given them some insights as to how these compounds might help in psychiatric disease.
Researchers started exploring the biological effects of psychedelics in the late 1990s, using neuroimaging techniques such as positron emission tomography5 before and after volunteers used the drugs, or in conjunction with antagonists that dampen some of their effects. The studies show similarities in how brains respond to psychedelics such as psilocybin and LSD, as well as to N,N-dimethyltryptamine (DMT), the active ingredient in ayahuasca, and to mescaline, a psychedelic compound derived from the peyote cactus. They all act on receptors for serotonin, a neurotransmitter that affects mood.
Serotonin is also the target of the predominant class of psychiatric drugs known as selective serotonin reuptake inhibitors, or SSRIs. It is now thought that these antidepressants work not by flooding the brain with the neurotransmitter, as was initially assumed, but by stimulating neuroplasticity — the brain’s ability to forge new neuronal connections. There is some evidence that psychedelic drugs, such as psilocybin, enhance neuroplasticity in animals6, and limited evidence suggests that the same might happen in human brains7,8. Clinical studies also suggest that the biological effects work best in concert with human guidance.
The setting for a psilocybin therapy session (shown in this mock-up) must be carefully replicated for clinical trials.Credit: COMPASS Pathways
The drugs “activate a therapeutic, dreamlike state, intensifying sensory perception, and memories pop up like little films”, says Franz Vollenweider, a psychiatrist and neurochemist at the University Hospital of Psychiatry in Zurich, Switzerland, and one of the pioneers of the modern era of psychedelic research. He thinks that this receptive state of mind provides an opportunity to help people escape from rigid patterns of thought, not unlike Rutter’s automatic circuit.
“People get locked into disorders like depression because they develop this system of thinking which is efficient, but wrong,” says David Nutt, a psychopharmacologist at Imperial College London and an outspoken supporter of evidence-based reforms to government policies concerning illegal drugs. Psychiatry has a term for such thinking: rumination. The idea behind psychedelic therapy is that the receptive state that the drug confers opens the door to fresh ideas about how to think about the past and future, which the therapist can reinforce. “There is a growing evidence base to the principle that this is very much about a synergy between drug-induced hyper-plasticity and therapeutic support,” says Carhart-Harris, who trained with Nutt.
Rutter says his journey with Carhart-Harris was focused, but flexible. When Rutter first removed a pair of eye shades after the drug took effect, the therapist appeared “fractured” and seemed to have another eye in the centre of his forehead. “I should imagine I look quite strange to you now,” Carhart-Harris said. Rutter burst out laughing and Carhart-Harris joined him. When the laughter stopped, the two men started talking. Rutter wanted to discuss his resentments, which led to pondering about the word ‘relent’ and its etymology. Carhart-Harris looked it up for him on his laptop. “That was a lovely moment, actually,” Rutter says. He returned for a second session with a stronger dose of the drug, followed by a second MRI and an ‘integration’ session, to discuss the experiences.
The treatment “made me look at grief differently”, Rutter says. “It was a realization that actually it wasn’t helping, and letting go wasn’t a betrayal.”
Clinical hurdles
Testing these drugs effectively and translating the clinical research into actual treatments will prove challenging, however. Two of the most closely watched studies have grappled with this. One is the recently completed MDMA trial, which was testing the approach in people with severe PTSD. It was a phase III study, usually the final stage before drug regulators decide whether to approve a treatment, and it involved 90 participants at 15 sites around the world. The Multidisciplinary Association for Psychedelic Studies (MAPS), a non-profit organization in San Jose, California, sponsored the study, but has not so far released the results.
Meanwhile, the mental-health-care company COMPASS Pathways in London is running a phase IIb trial — testing different dosages of psilocybin for treatment-resistant depression.
Evaluating the results won’t be simple. One concern revolves around controls. Most individuals given a placebo will know that they are not receiving a powerful hallucinogen. Some studies evaluating psychedelics have attempted to address this by giving people in the control group a pill containing niacin, which elicits a physical sensation — usually a flushing response in the skin. Mitchell says that some participants in her MDMA study who’ve been given the drug thought they received the placebo, while some taking the placebo believed that they had been given the drug.
The studies’ designers must also tackle how important the non-drug aspects of the trial are to the results. These include the mindset of the individual going into the experience, and the environment in which it takes place.
The vibe is definitely hotel spa at the treatment rooms for the COMPASS study at Utrecht University Medical Centre in the Netherlands. There’s a Mexican-style blanket folded at the foot of a twin-size bed. Beanbag chairs hug a potted palm in the corner. And a poster of Van Gogh’s Almond Blossom adorns one wall. All 24 sites in the study are similarly decorated.
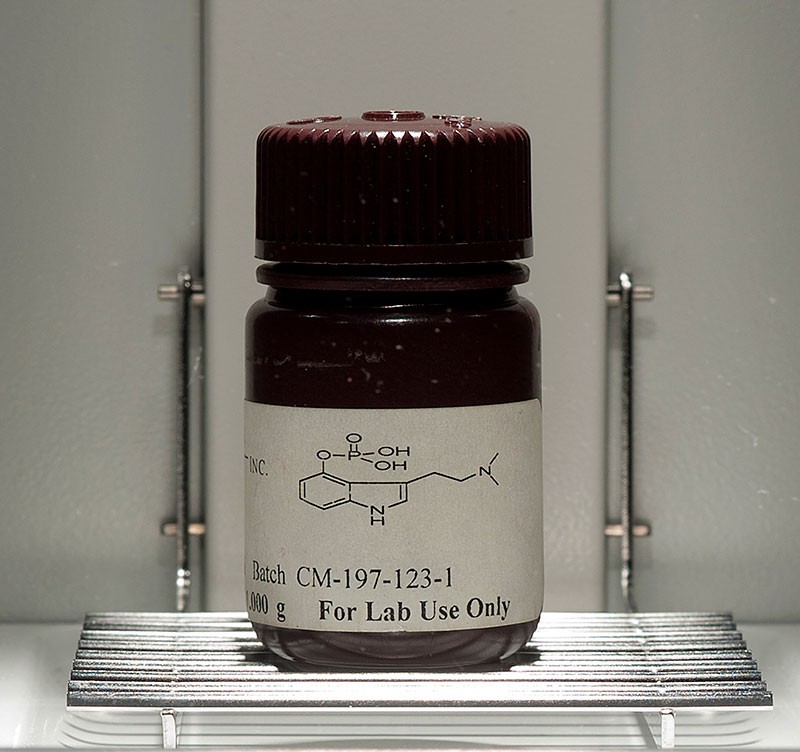
Synthetic psilocybin, the psychoactive ingredient found in magic mushrooms.Credit: Paul Taggart/Bloomberg/Getty
Then there’s the training and experience of the therapists guiding both the dosing sessions and the drug-free integration sessions. COMPASS, which became a public company in September and earned a stock-market valuation exceeding US$1 billion, developed a five-tier training programme for therapists in its trial. Company co-founder and chief innovation officer Ekaterina Malievskaia says site investigators must adhere to the training if the company expects to win regulators’ approval.
Madras goes further to say that the conditions of the trial will have to be replicated for any wider roll-out of the drugs. They “have to be approved under the stringent conditions in which they were investigated”, she says. But the path forward for mandating such conditions is unclear. For the US FDA, there is a mechanism to ensure that drugs are administered in a specific way: Risk Evaluation and Mitigation Strategies, or REMS. Through REMS, the agency can require prescribing physicians and pharmacists to be certified for a treatment strategy designed to mitigate the risks associated with a drug — such as addiction and dependency for opiate prescription. REMS could be used with psychedelics, Dunn says. The effect would be to bundle the delivery of the drug with the therapy component, and potentially certify practitioners. A source working on one of the trials says that discussions are under way with the FDA over whether therapists who administer the drugs ought to be trained, what that training might involve and whether therapist certification should be required.
Certification could mean legitimizing therapists who have been ‘treating’ individuals with the drugs illegally for as long as 30 years. But some of these therapists might resist the advice, or the involvement, of a government that has driven them underground.
Approvals still have a long way to go. Towards the end of 2020, MAPS reported in a news release that there are statistically significant differences in the response between the control and placebo groups in its MDMA trial (see go.nature.com/362xsvp). But the company won’t say more about the results until it releases the full data some time this year. It is also recruiting for a second phase III study using MDMA therapy for people with moderate-to-severe PTSD, which it aims to complete before the end of the year. COMPASS expects to have results from its phase IIb study on psilocybin by that time, and the company says it is planning a phase III study.
Robert Malenka, a psychiatrist and neuroscientist at Stanford University in California who has studied MDMA’s effects on rodents, says he thinks that some psychedelic drugs will eventually earn approval as treatments for certain conditions. “They have potential to be — I want to use the right analogy — a part of our toolset for treating patients,” he says. But he warns against overzealousness, particularly a brand of evangelism he’s seen among some of the underground purveyors of psychedelic-assisted psychotherapy. “I don’t think they’re going to be miracle cures,” he says.
He argues that the hypotheses for how the drugs might be working in the brain still need further research, and that investigating compounds that provide the same benefits without the hallucinatory effects could prove worthwhile in the long run. Others point out that SSRIs work for many individuals without clinicians fully understanding their mechanism.
Regarding the clinical work, however, Madras says she’s concerned by the studies’ size and design. She noted that many of them recruit people who have had previous experience taking psychedelics. Those who are attracted to this type of experience, she argues, might be more likely to say positive things about it. Nutt has said that working with experienced users of the drugs minimizes the chance of adverse events. But there are other potential confounders, according to Madras. “The consent forms tell you what the expectations are,” she says. “So there’s bias on the part of the subjects.”
Rutter says that despite all that, he is convinced that the treatment he received in 2015 changed his life for the better. In the weeks after his sessions, he found himself wondering whether the automatic circuit would return. “I was terrified,” he says, “and I realized I’ve got a little bit of control over this, right?” The thought had never occurred to him before.
A week or so later, he was out with friends at a shopping centre and sensed the return of optimism and openness. “It felt like somebody had opened a window in a stuffy room.” Five years later, his depression has not returned.
References
- Davis, A. K. et al. JAMA Psychiatry http://doi.org/10.1001/jamapsychiatry.2020.3285 (2020).
- Agin-Liebes, G. I. et al. J. Psychopharmacol. 34, 155–166 (2020).
- Carhart-Harris, R. L. et al. Psychopharmacology 235, 399–408 (2018).
- Vollenweider, F. X. & Preller, K. H. Nature Rev. Neurosci. 21, 611–624 (2020).
- Vollenweider, F. X. et al. Neuropsychopharmacology 16, 357–372 (1997).
- Zhang, G. et al. Neuropharmacology 64, 403–413 (2013).
- Hutten, N. R. P. W. et al. ACS Pharmacol. Transl. Sci. https://doi.org/10.1021/acsptsci.0c00099 (2020).
- Lebedev, A. V. et al. Hum. Brain Mapp. 37, 3203–3213 (2016).